Think about your body like a big world, and inside this world, there’s a strong army called the immune system. This army battles each day with germs, infections, and even tiny “bad cells,” which could turn into serious diseases. However, what’s interesting about this army is that it doesn’t go into battle directly. It requires signals, directions, and orders. One of the key “makers of signals” in this world is called Vitamin A.
In simple words,Vitamin A is an essential nutrient that plays a major role in keeping the body healthy. It supports normal vision (especially in low light), helps maintain healthy skin and body tissues, and is important for proper immune function.
But here’s where the story becomes shocking and interesting. Sometimes, smart enemies don’t fight with powerful cells—they fight with tricks. New research suggests that in certain situations, a Vitamin A byproduct may actually help cancer cells hide, like someone hiding in the dark.Instead of helping the immune system spot the cancer, this Vitamin A pathway can slowly weaken immune cells and make them less active—like the body’s guards become sleepy and stop watching, so the danger can slip in without being noticed.
Table of Contents
ToggleSource of this information:
This information comes from an official research news/press release published by the Ludwig Institute for Cancer Research (Princeton Branch), where scientists explained how a Vitamin A byproduct (all-trans retinoic acid) can weaken immune defenses.
Quick Summary:
Vitamin A is important for vision and immunity, but a byproduct called retinoic acid can be misused by tumors to “hide” from the immune system and weaken T-cell attack.
What Scientists Reveal:Vitamin A May Help Cancer Hide From Immunity
The scientists discovered that a Vitamin A-derived molecule called All-Trans Retinoic Acid(also known as retinoic acid).Vitamin A itself isn’t bad -The real issue is a molecule made from it.
This molecule is produced inside the body and acts like a signal messenger. Think of it like a “command note” that tells cells what to do.
In healthy situations—especially in your gut—retinoic acid helps prevent the immune system from overreacting. It helps keep inflammation under control.
But cancer is clever. Tumors learn how to use this same signal to create something called immune tolerance—basically, making the immune system too calm and too forgiving around the tumor.
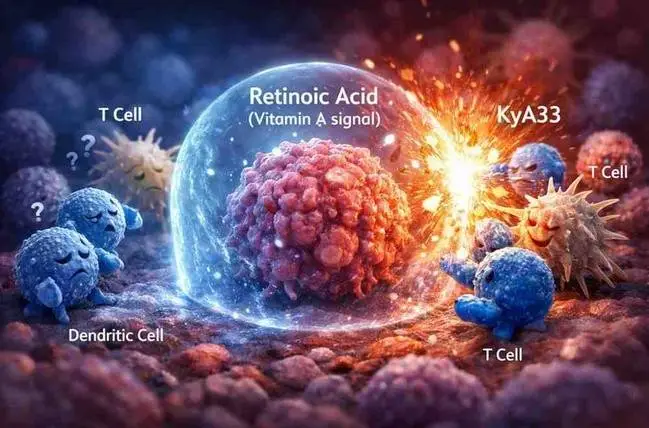
The Immune System Has Soldiers… But Tumors Use Retinoic Acid Like a Smoke Screen
Think of your immune system like an army that protects your body.Inside this army are strong fighters called T cells. Their job is simple:
find danger and destroy it — including cancer cells.But tumor cells are not easily affected by the immune system.
So what do they do?
They create an environment where immune cells become confused, tired, or inactive. Retinoic acid seems to help tumors build this environment—almost like putting a fog/smoke screen around themselves.
This means the immune system may fail to recognize the tumor as a serious threat, and the body may respond as if, “This is not dangerous. It can be ignored.”
This is extremely dangerous because when cancer is not detected and attacked early, it gets time to grow, spread, and become harder to treat.
Dendritic cells and Cancer immunity
The research focuses on a very important immune cell:
Dendritic Cells (DCs) : Dendritic cells are like the teachers of the immune system.
They don’t directly fight like soldiers. Instead, they:
Detect danger (cancer or infection).
Collect pieces of the threat (antigens).
Show those pieces to T cells.
Train T cells to attack.
What Are Dendritic Cell Vaccines and How Are They Made?
Dendritic cells are like the teachers of the immune system. They don’t fight directly, but they guide other immune cells—especially T cells—by showing them what to attack. To make a DC vaccine, doctors and scientists first collect immune cells from a patient. Then in a lab, they carefully grow and turn them into dendritic cells. After that, they “train” these dendritic cells using tiny pieces of the patient’s tumor, so they learn what the cancer looks like. Finally, these trained dendritic cells are injected back into the patient, with the goal of triggering a strong immune attack against the tumor.
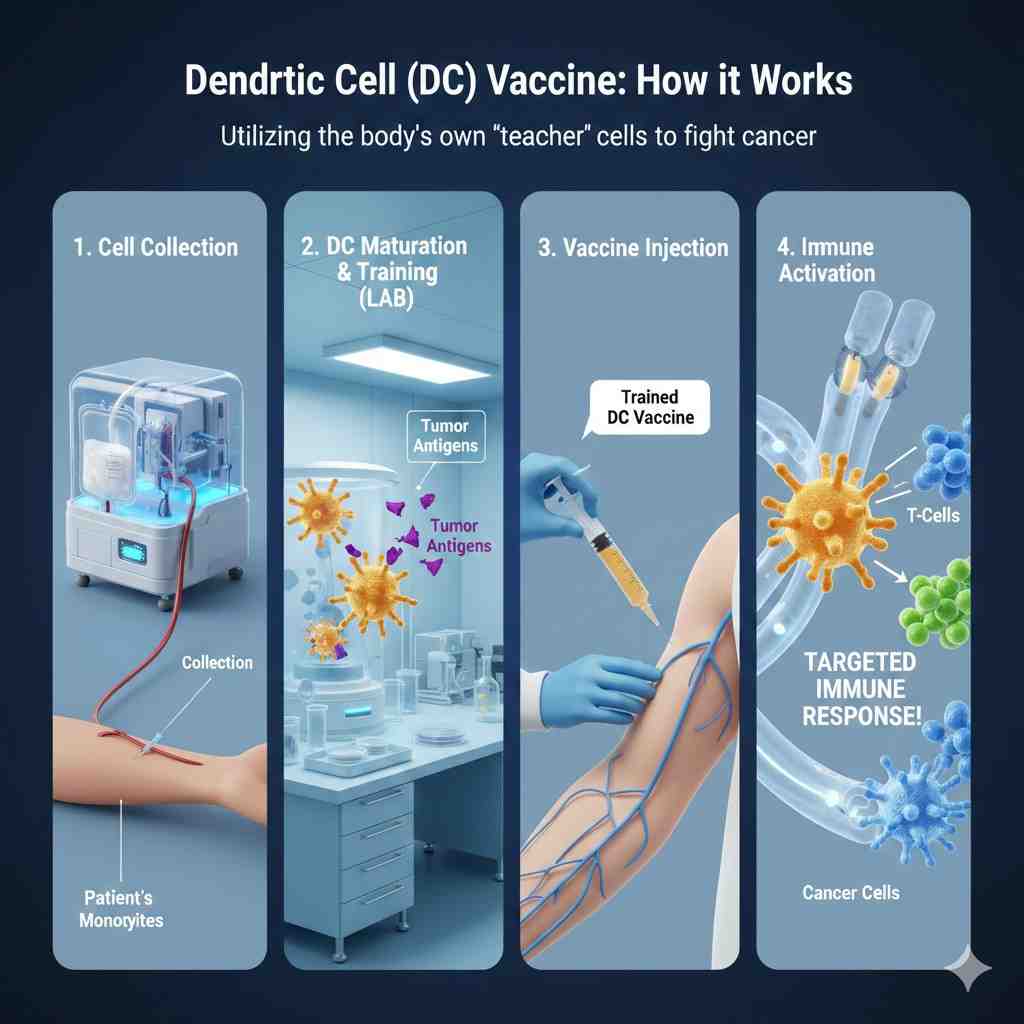
The Shocking Discovery: Why Some Cancer Vaccines Become Weak Before They Even Start
This was the part that truly surprised scientists. There is a special type of immunotherapy called Dendritic Cell (DC) Vaccines. These vaccines are designed to train your immune system to recognize cancer and destroy it, almost like teaching your body’s soldiers to identify an enemy properly. The idea sounds powerful, and it is—but in real life, many DC vaccines have not worked as well as expected. Researchers wanted to understand one big question: Why do these vaccines fail even when the science looks correct?
The Hidden Problem: Vaccine-Making Conditions Can Trigger Immune Weakening
Here’s what researchers discovered that changed everything. During the lab process—while dendritic cells are being prepared for the vaccine—the conditions used can accidentally push the cells into producing something called retinoic acid, which is a Vitamin A byproduct. Instead of making the dendritic cells stronger, this retinoic acid does the opposite. It prevents dendritic cells from maturing properly, and immature dendritic cells cannot teach T cells well. So the vaccine becomes weak, not because the idea is wrong, but because the vaccine cells get “softened” before they even enter the body.
This finding is important because it may explain why many dendritic cell vaccines have shown disappointing results in clinical trials. In simple words: the vaccine cells may lose their power during the manufacturing process itself.
The Enzyme Behind the Problem: ALDH1a2 and ALDH1a3
Retinoic acid doesn’t appear randomly—it’s created by specific enzymes. Two major ones are ALDH1a2 and ALDH1a3. ALDH1a2 is found in certain dendritic cells and can trigger retinoic acid production during vaccine preparation. ALDH1a3 is especially important because it is often found at high levels inside cancer cells. When these enzymes are more active than normal, retinoic acid increases, and immune becomes weakening become stronger.
Even more worrying, many tumors show very high ALDH1a3 levels, and studies link this with worse survival outcomes across multiple cancers. That means some cancers may be using ALDH1a3 almost like a weapon to protect themselves from immune attack.
The Breakthrough Drug: KyA33 (The “Off Switch”)
Now comes the hopeful part. Scientists developed an experimental drug called KyA33. You can think of it like an “off switch” for the retinoic acid pathway. This drug can block retinoic acid production and prevent immune suppression from happening. It helps dendritic cells mature properly again, so they can train T cells effectively. This means DC vaccines become stronger and more successful.
In mouse studies of melanoma, DC vaccines prepared in the presence of KyA33 created a much stronger immune response. Tumors grew slower and cancer progression reduced. Even more exciting, KyA33 also worked as a stand-alone immunotherapy, meaning it could help the immune system fight cancer even without being used inside a vaccine.
Why This Discovery Is a Big Deal for Cancer Treatment
This discovery is exciting because it opens a completely new direction in cancer immunotherapy. Most current immune-based cancer treatments focus on methods like checkpoint inhibitors, CAR-T therapy, and monoclonal antibodies. These treatments mainly work by boosting immune cells or removing brakes from them. But KyA33 targets something different and very important: it blocks the tumor’s ability to create immune tolerance.
In simple words, instead of only strengthening the immune system, this approach removes the “invisibility cloak” tumors use to hide. And if tumors cannot hide anymore, other immunotherapies may work better too.
What This Means for Normal People: Should You Stop Taking Vitamin A?
No, you should not panic or suddenly stop Vitamin A completely. Vitamin A is essential for normal health. Your body needs it for vision, immunity, skin health, and growth. But this research is a strong reminder that too much Vitamin A—especially from high-dose supplements—may not be safe.
Cancer biology is complicated, and “more vitamins” doesn’t always mean “more protection.” The safest rule is simple: get Vitamin A mostly from natural foods like carrots, spinach, eggs, milk, and dairy products. Avoid high-dose Vitamin A supplements unless a doctor specifically recommends them.
Conclusion:
Vitamin A isn’t the enemy. It’s a normal part of how the body functions. But cancer is a master of manipulation. This research shows tumors may use retinoic acid signals to weaken dendritic cells, reduce vaccine success, slow immune attacks, and remain hidden. That’ssurprising—but also powerful knowledge.